Opioid-Sparing Enhanced Recovery After Surgery (ERAS) Protocol for Lumpectomy Patients Results in Improved Postoperative Pain Control
Submitter
Claudya Morin MD
Claudya Morin MD, Munazza Javid MD, Yamini Patel MD, Peter Flom PhD, Charusheela Andaz MD, Donna Marie Manasseh MD, Patrick I. Borgen MD, Kristin Rojas MD
Objectives
Our previous pilot study found that an opioid-sparing Enhanced Recovery After Surgery (ERAS) protocol was feasible. In the present study, we sought to demonstrate a clinically significant reduction in postoperative pain through a comparison to a large historical cohort.
Methods
A prospective cohort of patients undergoing lumpectomy with varied axillary management received an opioid-sparing ERAS protocol. In-hospital and discharge opioids were compared to a historical cohort that received usual care (non-ERAS) using oral morphine equivalents (OMEs). Postoperative day one and week one pain scores were compared using Kruskal-Wallis test.
Results
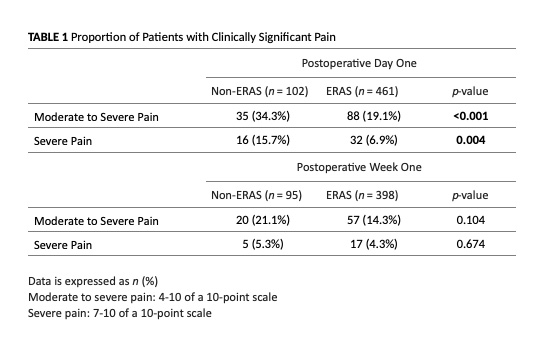
Between 2017 and 2019, 729 patients received the ERAS protocol and were compared to a similar historical control group of 624 patients who underwent surgery between 2015 and 2018. Of the ERAS patients, 634 underwent lumpectomy with varied axillary management. Median pain scores were significantly lower in the ERAS group when compared to the non-ERAS group both the day after surgery (2 vs. 0, p <0.001) and the week after surgery (1 vs. 0, p<0.001). Furthermore, ERAS patients were significantly less likely to report severe pain (7-10 of 10-point scale) on the day after surgery when compared to non-ERAS patients (15.7% vs. 6.9%, p=0.004). Patients in the ERAS group were discharged with a median of 0 OMEs (range 0-150), while the non-ERAS group were discharged with a median of 90 OMEs (range 0-360) (p<0.001).
Conclusion Implication
Postoperative prescriptions play a major role in the opioid crisis. We found that implementation of an opioid-sparing ERAS protocol in patients undergoing lumpectomy resulted in significantly improved postoperative pain scores without the routine prescription of postoperative opioids. Surgeons can improve their own patients’ outcomes while addressing the larger societal issue of the opioid crisis by adopting similar protocols that decrease the quantity of opioids available for diversion within our patients’ communities.